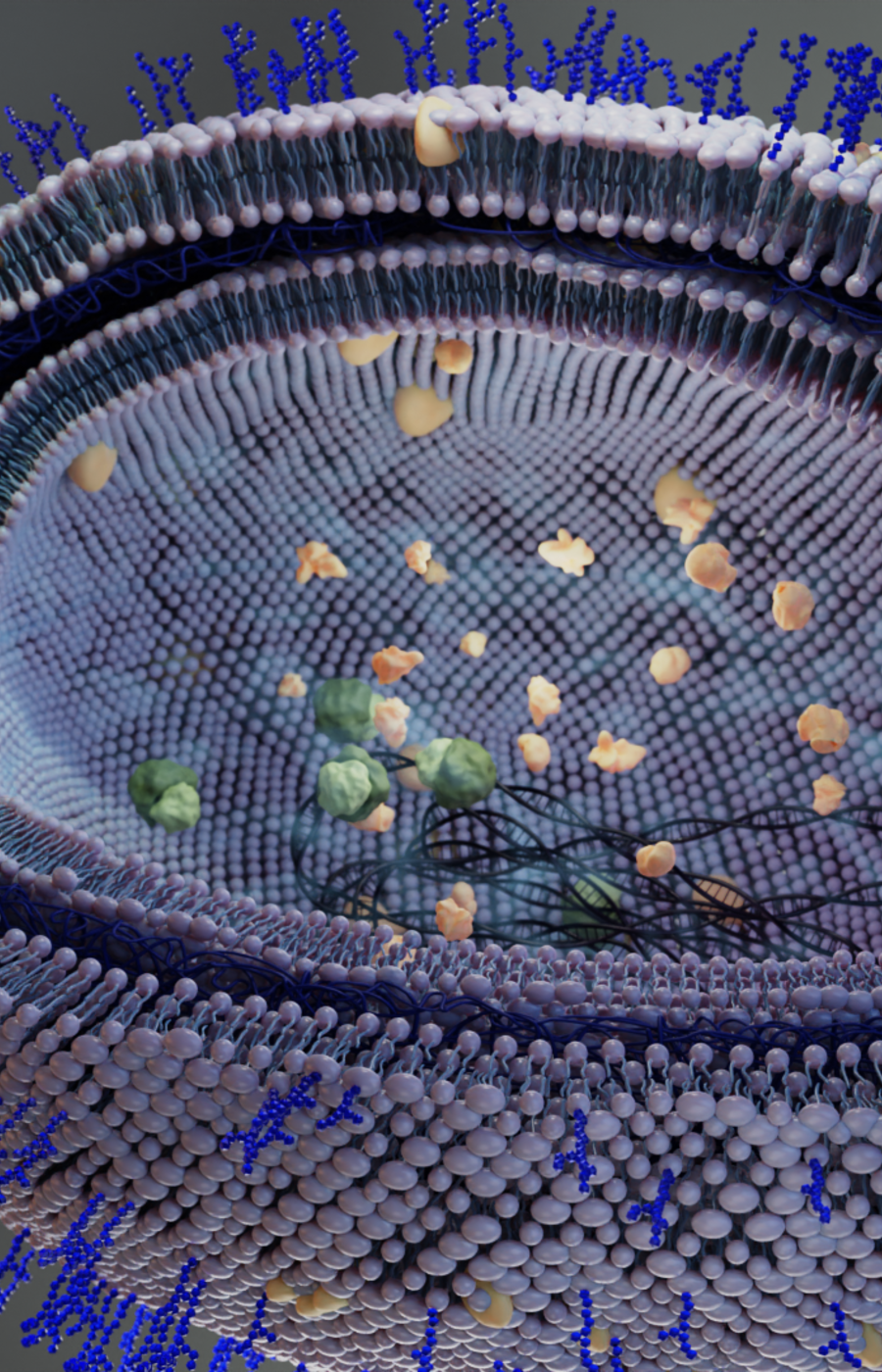
According to research published in The Lancet in January 2022, antimicrobial resistance was directly responsible for the deaths of 1.27 million people in 2019, and by some estimates, this number could rise to 10 million deaths per year by 2050. ‘The spread of antimicrobial resistance is outpacing almost every countermeasure, and the world has limited choices to treat infections,’ warn Katia Iskandar of the University of Toulouse and colleagues in a 2022 review paper in the journal Antibiotics.
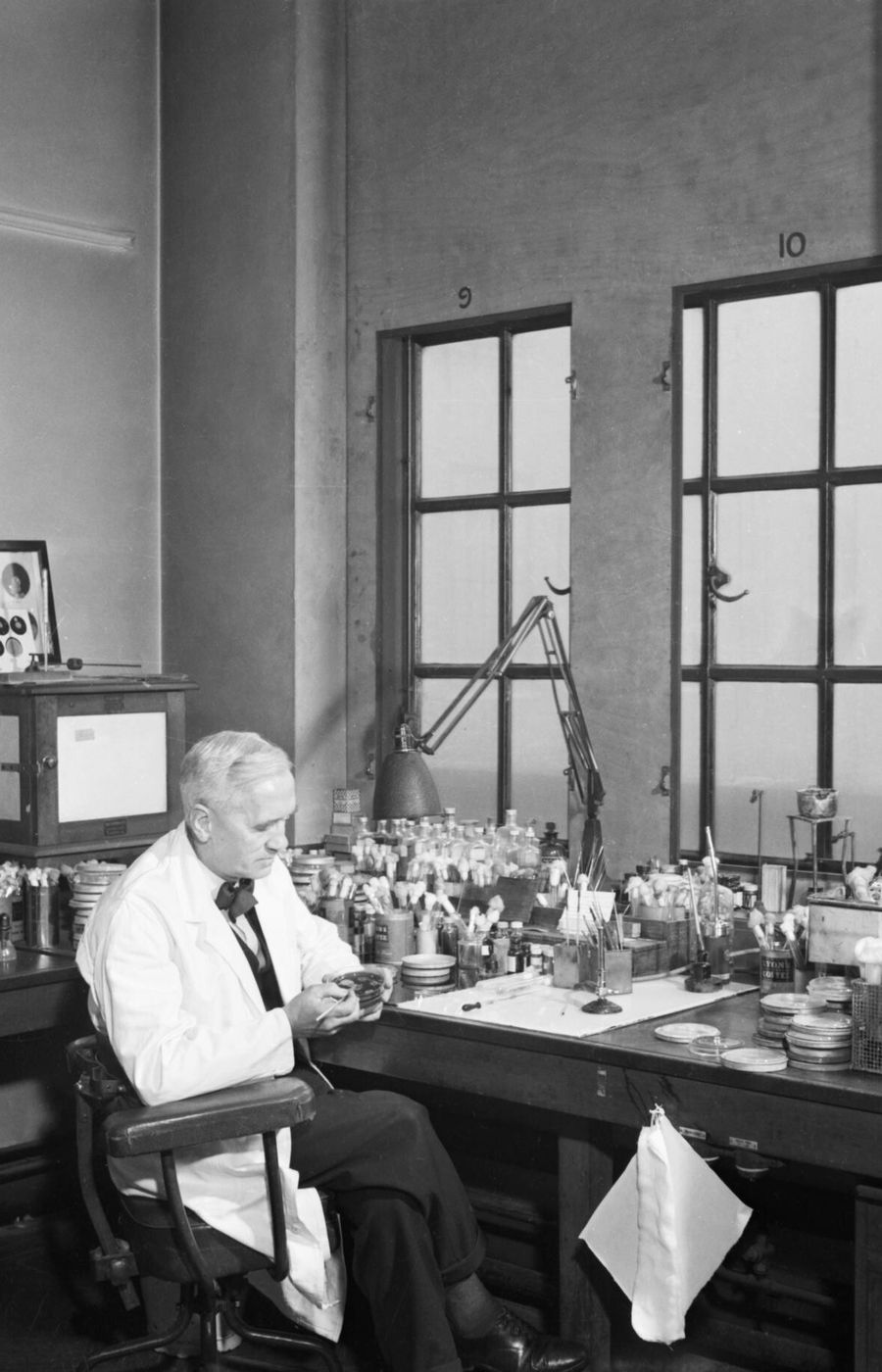
How has this happened? The problem is far trickier than Fleming predicted – and it can’t simply be blamed on negligent Mr X. The medical establishment, drug companies and governments have all played a role.
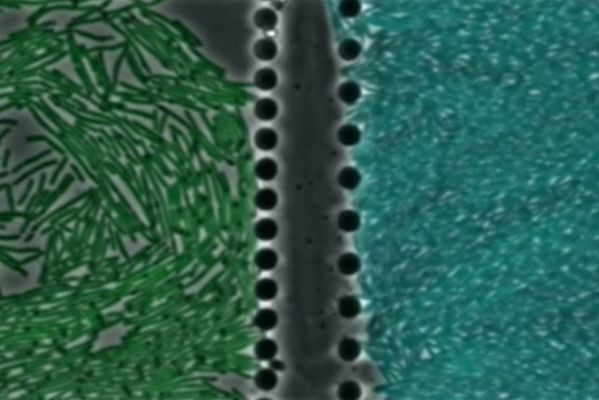
‘It's kind of an arms race between bacteria and the development of new treatments,’ explains Jonkergouw. But sadly, it’s a race we’re losing. As antibiotic-resistant encounters have risen rapidly, the development of novel therapies has fallen far behind. The number of new antibiotics in trials – as tracked by the World Health Organization – is worryingly small.
‘The traditional business model for antibiotic research and development is broken,’ write Silke Alt of the German Center for Infection Research (DZIF) and colleagues in a recent comment piece in Nature Reviews Drug Discovery.
How so? Most obviously, ‘it's expensive to make a new drug,’ explains Douglas Häggström of INCATE, the INCubator for Antibacterial Therapies in Europe, which helps universities commercialise research to tackle the antimicrobial resistance problem. But it's more complex than just the cost alone.
Companies knows that even if a new antibiotic makes it through expensive clinical trials, nowadays doctors may use it only as a treatment of last resort. ‘Because resistance develops at a population level, you don't want to prescribe these drugs very often,’ Häggström explains. Ten years later, the patent expires, and the company’s hope of recouping their investment dries up.